Worried About the Correct Diagnosis for Anal Fistula?
VAAFT Treatment in Navi Mumbai
Advanced VAAFT (Video Assisted Anal Fistula Treatment) in Navi Mumbai
- Dr Nitish Jhawar, with 23 years of experience
Book An Appointment
What is VAAFT?
VAAFT, or Video-Assisted Anal Fistula Treatment, is an innovative, minimally invasive and sphincter saving technique to treat complex anal fistulas with precision and minimal disruption to surrounding tissue.Dr Nitish Jhawar is internationally trained in VAAFT by the inventor of the technique Dr P. Meinero himslef,.
To understand it better, think of treating an anal fistula as fixing a leak in a network of underground pipes. In the past, fixing these leaks meant digging large holes in the ground, causing damage to the area around it. Similarly, traditional fistula surgery often involved large cuts, which increased recovery time and risked damaging important muscles (anal sphincters) that help control bowel movements.
With VAAFT:
- A tiny camera (like an inspection tool for pipes) is inserted, allowing the surgeon to see the full fistula tract without large incisions.
- This camera-guided approach helps the surgeon precisely target and treat the fistula, sparing healthy tissue and preserving the sphincter muscles.
- The result? Less pain, faster recovery, and a reduced risk of incontinence (loss of bowel control), as the muscles are left intact.
In short, VAAFT enables the surgeon to treat fistulas accurately, protecting muscle function and allowing patients to recover quickly and comfortably.
Understanding Anal Fistula and the Need for VAAFT
Overview of Anal Fistula
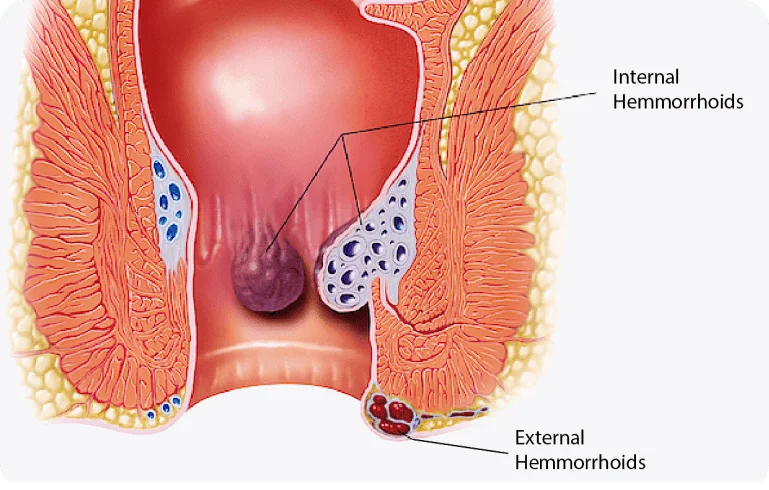
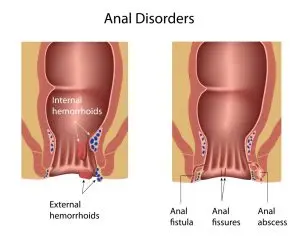
An anal fistula is an abnormal tunnel that forms between the inside of the anus or rectum and the skin around the anus. This condition often develops as a result of an infected anal gland that creates an abscess. When the abscess doesn’t heal properly, it can create a persistent tunnel, leading to discomfort, pain, and sometimes discharge.
Symptoms of Anal Fistula Include:
- Pain, especially during bowel movements
- Swelling or tenderness around the anus
- Discharge of pus or blood
- Irritation or itching
Anal fistulas come in various forms:
- Simple Fistulas – Straightforward paths from the anus to the skin.
- Complex Fistulas – More branching tracts that may extend deeper or curve, making treatment more difficult.
- Recurrent Fistulas – Fistulas that reappear after previous treatments.
For more challenging cases, like complex or recurrent fistulas, a precise, minimally invasive approach is often required, which is where VAAFT (Video-Assisted Anal Fistula Treatment) offers significant benefits.
Diagnosis of Anal abscess and fistula
Digital rectal examination is an important step in the evaluation anal fistula.
Sigmoidoscopy may be required to locate the internal opening and to check for any other issues.
Sometimes colonoscopy may be done for patients with recurrent anal fistula with symptoms of inflammatory bowel disease.
Endoanal ultrasonography is useful in the total assessment of anal fistula.
Fistulography and magnetic resonance imaging may be useful for complex recurrent anal fistula.
Traditional Fistula Treatments vs. VAAFT
Traditionally, treatments for anal fistulas often involved procedures like fistulotomy or open surgery. These methods require larger incisions, increasing the risk of injury to surrounding tissues, including the anal sphincters (muscles that help control bowel movements). Damage to these muscles can lead to complications, including incontinence.

VAAFT, however, uses a small camera to guide the surgeon through the fistula tract, enabling precise and less invasive treatment. This approach significantly lowers the risk of sphincter damage, speeds up recovery, and reduces post-operative pain.
Here’s a simplified comparison between traditional treatments and VAAFT:
Aspect | Before VAAFT: Traditional Treatment | With VAAFT |
Visualization | Limited view, requiring larger incisions for access. | Clear, magnified view using a camera for precise targeting. |
Invasiveness | More invasive, with large cuts, leading to longer recovery times. | Minimally invasive, using small incisions, reducing pain. |
Sphincter Preservation | Higher risk of damaging anal sphincters, potentially causing incontinence. | Better sphincter preservation, minimizing incontinence risk. |
Recovery Time | Longer recovery with more discomfort and longer hospital stays. | Faster recovery, less pain, and often shorter hospital stays. |
Risk of Recurrence | Higher if fistula tracts aren’t fully visualized or treated. | Lower recurrence due to thorough, targeted treatment. |
Why Traditional Treatments May Not Be Effective for Complex or Recurrent Fistulas
In cases of complex or recurrent anal fistulas, traditional treatments like fistulotomy or open surgery often fall short. Here’s why:
Limited Visualization:
- Traditional methods don’t offer the detailed visualization needed to navigate through the intricate paths of complex or branching fistulas. Surgeons often rely on physical examination and imaging, which can miss smaller branches or deeper extensions.
- This limited view increases the risk of incomplete treatment, which can leave parts of the fistula untreated, leading to higher chances of recurrence.
More Invasive Approach:
- Treating complex fistulas with traditional surgery requires larger incisions to reach the full tract. This can lead to more tissue damage, prolonged healing times, and a higher likelihood of infection.
- In cases of recurrent fistulas, each surgery weakens surrounding tissues, making it harder to achieve a durable solution with every subsequent procedure.
Sphincter Involvement:
- Complex and recurrent fistulas often run close to or through the anal sphincters (internal and external muscles that control bowel movements). Traditional methods may involve cutting through or near these muscles to access and remove the fistula tract, which raises serious risks.
Risk of Damaging the Anal Sphincters
The internal and external anal sphincters are critical for bowel control, acting like muscles that close tightly to prevent unwanted bowel leakage. Damage to these muscles during traditional fistula surgery can have lasting impacts:
- Incontinence: When the sphincters are injured, patients may experience faecal incontinence (loss of control over bowel movements). This can range from minor leakage to complete inability to control bowel movements, which greatly affects the patient’s quality of life.
- Nerve Damage: Surgical procedures around the sphincters may also inadvertently harm nearby nerves, further compromising muscle function and sensation.
- Longer Recovery and Functional Loss: Even if sphincter damage doesn’t lead to immediate incontinence, it can reduce muscle strength and function over time, affecting the stability and control of bowel movements.
How VAAFT Minimizes These Risks
With Video-Assisted Anal Fistula Treatment (VAAFT), the surgeon uses a camera to navigate the entire fistula tract with precision. This allows them to target and treat the fistula without making large incisions or disturbing the anal sphincters. VAAFT significantly reduces the risk of:
- Incomplete Treatment: The camera provides a complete view of the fistula, ensuring no part is left untreated, lowering the risk of recurrence.
- Sphincter Damage: The minimally invasive approach helps avoid cutting near or through the sphincters, preserving their integrity and function.
In summary, VAAFT’s precise and minimally invasive approach is particularly beneficial for complex and recurrent anal fistulas, as it allows effective treatment while protecting the sphincter muscles and reducing recovery time.
Other Potential Applications of VAAFT in Colorectal Surgery
Pilonidal Sinus Surgery
- VAAFT can be adapted to treat pilonidal sinus disease, a condition where hair follicles become infected near the tailbone
- The video-assisted approach allows for precise removal of the sinus tract and reduces recurrence compared to open surgery.
Intersphincteric Abscess Drainage
- In cases of intersphincteric abscesses, video-assisted approaches can be utilized for precise drainage, reducing the risk of recurrence and improving recovery.
Complex or Recurrent Fistulas
- VAAFT can be particularly useful for treating recurrent fistulas, especially those with complex tracts or extensions that are difficult to access with traditional methods.
- Video guidance allows for better identification and closure of the fistula path.
Treatment of Anal Fissures
- VAAFT can sometimes assist in procedures for chronic anal fissures that require surgical intervention.
- The visual precision aids in sparing surrounding tissue and achieving more targeted treatment.
Perianal Crohn's Disease
- Video-assisted techniques help manage fistulas and abscesses in patients with Crohn's disease, particularly when other surgical approaches have higher risks.
- VAAFT allows for careful management of these complex cases, reducing complications.
How Is VAAFT Treatment Done?
Step-by-Step Guide
- Pre-Operative Steps: Before the procedure, you’ll consult with the surgeon to discuss your medical history and review imaging studies (like MRI or ultrasound) to map out the fistula.
- Anaesthesia: The VAAFT procedure is typically performed under general or spinal anaesthesia to keep you comfortable and pain-free throughout the surgery.
- Procedure :
- A tiny camera (endoscope) is inserted into the fistula tract to provide a clear, magnified view.
- The surgeon carefully examines the entire tract, identifying any branching paths.
- The fistula tract is then treated with precise techniques to close it off without harming nearby muscles, especially the sphincters.
- Closure and Recovery: Once the tract is treated, it’s sealed, and minimal incisions are closed.
What to Expect
- Duration: The VAAFT procedure generally lasts between 30 minutes and an hour, depending on the complexity of the fistula.
- Recovery Timeline: Most patients experience mild discomfort post-surgery, typically subsiding within a few days. Full recovery and return to normal activities generally take 1-2 weeks, with a follow-up visit to monitor healing.
Post-Procedure Care and Recovery
Immediate Aftercare
- Wound Care: Keep the area clean and dry, and follow your surgeon's instructions for wound care.
- Hot Sitz bath :Soak the affected area in warm water for 10-15 minutes, 2-3 times a day, to ease pain, promote healing, and keep the area clean. Avoid adding any substances unless recommended by your doctor.
- Managing Discomfort: Mild pain or discomfort is normal; pain relievers may be prescribed to ease any post-surgery soreness.
- Rest: Limit physical activity for a few days to allow the area to heal and reduce swelling.
Long-Term Recovery and Follow-Up
- Resuming Activities: Most patients can return to normal daily activities within 1-2 weeks, though strenuous activities should be avoided until cleared by the doctor.
- Follow-Up Visits: Follow-up appointments are essential to monitor healing, ensure the fistula has closed properly, and check for any signs of recurrence.
Regular follow-ups support a smooth recovery and allow early intervention if any issues arise.
Frequently Asked Questions (FAQ) on VAAFT
VAAFT is suitable for patients with complex or recurrent anal fistulas, especially those close to the anal sphincters. It’s recommended for individuals seeking a minimally invasive solution with a lower risk of incontinence.
VAAFT is considered a safe and effective treatment for anal fistulas. Its minimally invasive nature means a lower risk of complications compared to traditional methods, with reduced chances of damage to the anal sphincters.
While no procedure can guarantee zero recurrence, VAAFT’s precision significantly lowers the chances of fistula recurrence. Follow-up care and proper wound management further help reduce this risk.
VAAFT is typically performed under general or spinal anaesthesia, ensuring that the patient is comfortable and pain-free during the procedure.
VAAFT has a high success rate, especially for complex and recurrent fistulas, as it enables complete visualization and targeted treatment of the fistula tract. Outcomes are typically very positive, with a high healing rate and low risk of complications.
Most patients can resume light activities within a few days and return to work within 1-2 weeks, depending on the nature of their job and individual recovery speed.
